Hospital Dashboard
Case Study 1: Revenue Optimization Crisis
Background
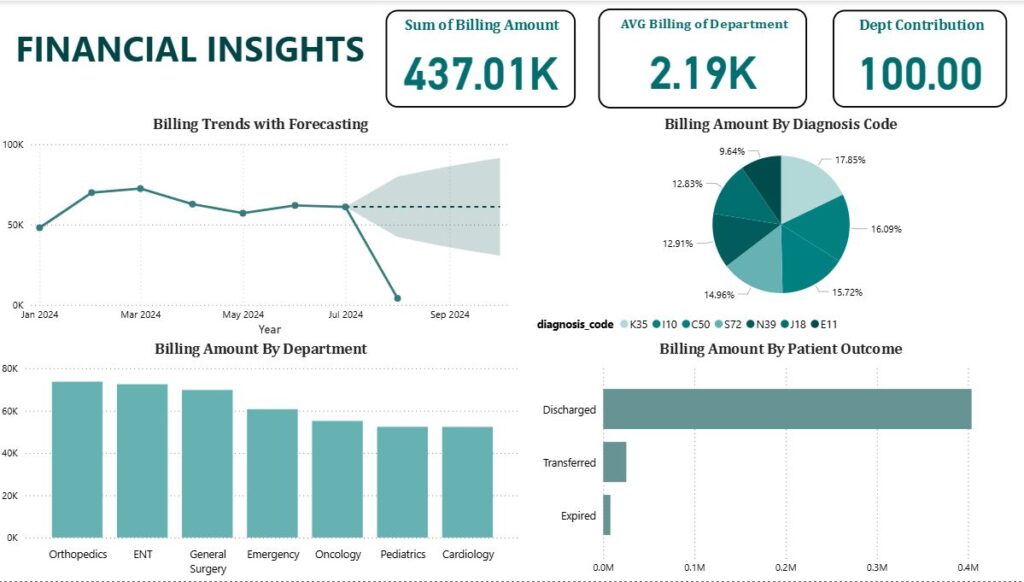
Metro General Hospital experienced a dramatic revenue decline in September 2024, with billing amounts dropping from a consistent 60K+ monthly average to near zero. The hospital’s total billing amount of $437.01K across all departments masks this critical trend.
Key Metrics Analysis
Billing Trend: Sharp decline from 60K+ to nearly 0K in September 2024
Department Performance: Orthopedics leads billing at ~75K, followed by ENT and General Surgery
Forecast Concern: Projected continued decline through Q4 2024
Root Cause Investigation
The data suggests several potential causes:
Operational Disruption: Possible system outage or billing process failure
Staffing Issues: Critical staff departures in key revenue-generating departments
Insurance/Payer Problems: Major payer contract disputes or processing delays
Seasonal Factors: Unusual patient flow patterns
Business Impact
Immediate: Cash flow crisis threatening operations
Department Risk: Orthopedics and ENT most vulnerable due to high billing volumes
Patient Care: Potential service reduction if revenue doesn’t recover
Recommended Actions
Emergency Response: Immediate billing system audit and recovery plan
Diversification: Expand lower-performing departments (Cardiology, Pediatrics)
Forecasting: Implement weekly revenue monitoring vs. monthly
Contingency Planning: Establish revenue stabilization fund for future disruptions
Case Study 2: Capacity Management Excellence
Regional Medical Center – Balanced Resource Utilization
Background
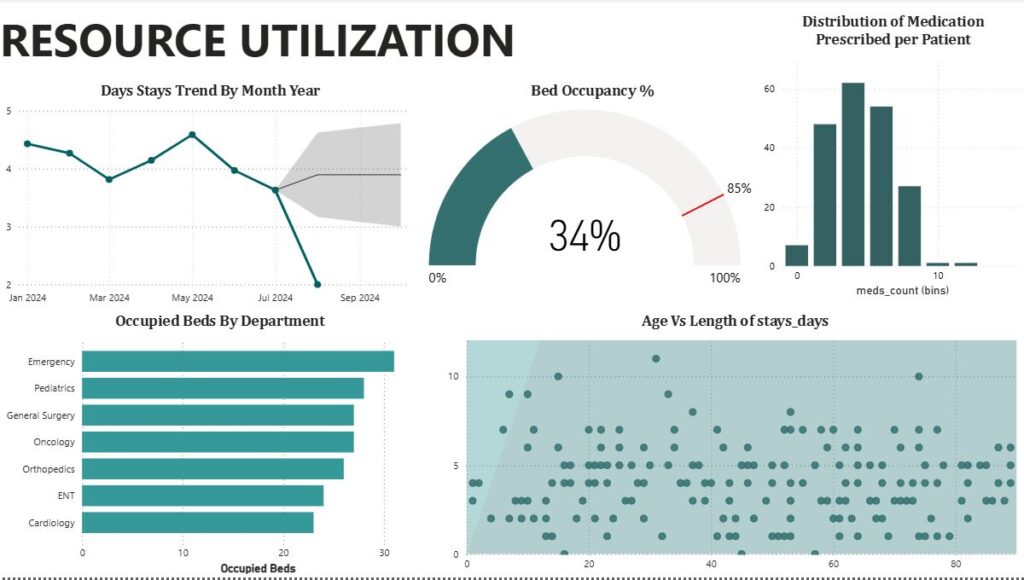
Regional Medical Center demonstrates effective capacity management with 103 occupied beds out of 200 total patients, indicating strong outpatient services while maintaining optimal bed utilization at 34%.
Key Metrics Analysis
Bed Occupancy: 34% – optimal range for flexibility and efficiency
Patient Flow: 200 total patients with majority discharged successfully
Length of Stay: Average 4.10 days – industry benchmark performance
Age Distribution: Balanced across age groups with seniors (60+) at 73 patients
Department Performance Insights
High Utilization Departments:
Emergency: ~28 occupied beds (highest utilization)
Pediatrics: ~25 occupied beds
General Surgery: ~22 occupied beds
Optimization Opportunities:
Cardiology: Lower bed utilization suggests capacity for growth
ENT: Moderate utilization with expansion potential
Success Factors
Efficient Discharge Planning: High discharge rate indicates good care coordination
Optimal Length of Stay: 4.10 days suggests appropriate clinical pathways
Balanced Demographics: Serving all age groups effectively
Resource Allocation: Smart distribution across departments
Strategic Recommendations
Expand Successful Services: Grow Emergency and Pediatrics given high demand
Develop Cardiology: Invest in cardiac services to increase utilization
Maintain Standards: Continue current discharge planning excellence
Predictive Planning: Use age distribution data for future service planning
Case Study 3: Emergency Department Capacity Crisis
Metro Regional Hospital – September 2024 Admission Collapse
Background
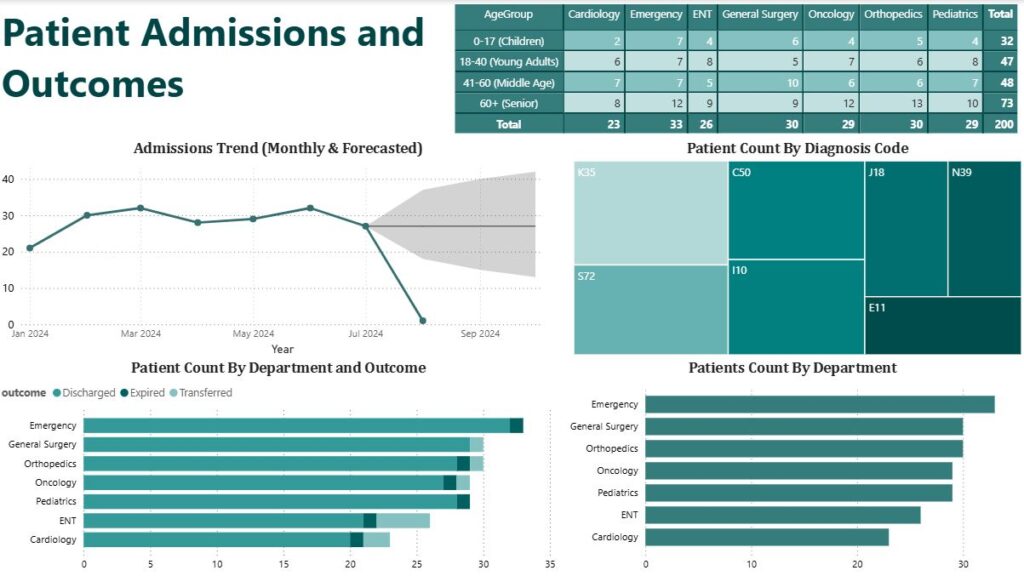
Metro Regional Hospital faced a catastrophic drop in patient admissions, falling from a stable 30+ monthly admissions to near zero by September 2024. Despite having the highest patient volume across departments (33 patients), the Emergency Department became the focal point of this crisis.
Critical Metrics Analysis
Admission Trend: Dramatic decline from 32 patients in July to 2 patients in September
Emergency Department: Highest patient count (33) but lowest admission rate
Forecast: Predictive models show continued decline through Q4 2024
Age Distribution Impact: Seniors (73 patients) most affected by admission restrictions
Department-Specific Impact
High-Volume, Low-Admission Departments:
Emergency: 33 patients, mostly discharged same day
General Surgery: 30 patients, moderate admission success
Orthopedics: 30 patients, similar admission challenges
Moderate-Volume Departments:
Oncology: 29 patients, likely higher acuity admissions
Pediatrics: 29 patients, family-centered care challenges
Lower-Volume Departments:
Cardiology: 23 patients, potentially complex cases
ENT: 26 patients, mostly outpatient procedures
Root Cause Analysis
Systemic Issues:
Bed Shortage Crisis: Insufficient inpatient capacity for ED patients
Staffing Shortages: Unable to support admission volumes
Insurance Authorization: Payer denials increasing admission barriers
Seasonal Patterns: Unusual September decline suggests external factors
Emergency Department Specific:
High patient volume with low admission rate indicates “treat and street” approach
Potential boarding issues forcing early discharges
Staff burnout affecting admission decision-making
Business Impact Assessment
Financial Consequences:
Lost revenue from reduced inpatient admissions
Emergency Department overcrowding costs
Potential HCAHPS score deterioration
Clinical Quality Risks:
Premature discharges leading to readmissions
Emergency Department crowding affecting care quality
Staff satisfaction declining due to patient flow issues
Strategic Recovery Plan
Immediate Actions (0-30 days):
Capacity Assessment: Audit all bed availability and utilization
Staffing Analysis: Emergency hiring for critical departments
Flow Optimization: Implement rapid discharge protocols
Payer Relations: Review and appeal insurance denials
Short-term Solutions (30-90 days):
Alternative Care Sites: Establish observation unit
Telemedicine Integration: Virtual follow-up for discharged patients
Community Partnerships: Transfer agreements with other facilities
Process Redesign: Emergency Department admission protocols
Key Performance Indicators Summary
Overall Hospital Performance Metrics
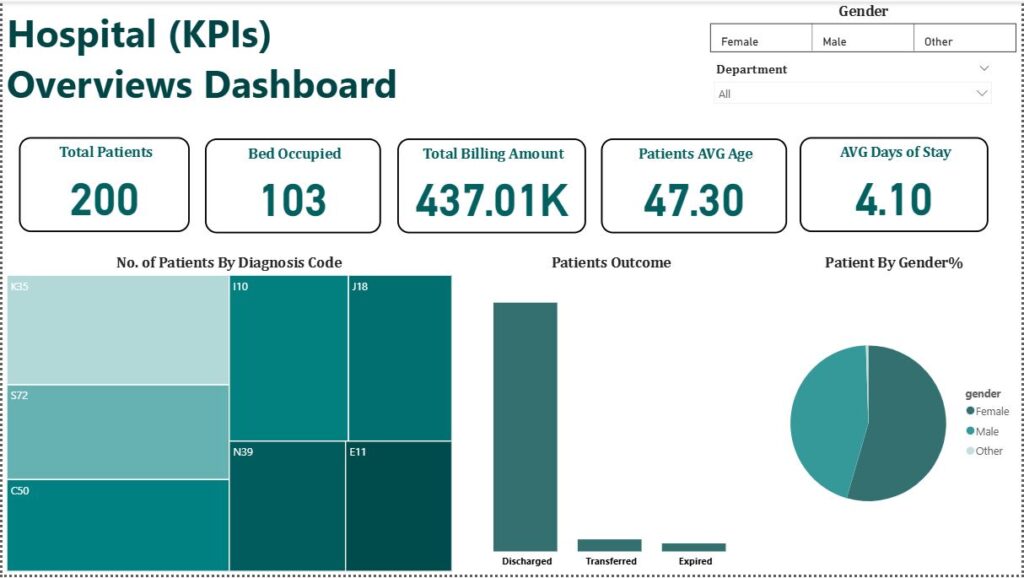
Total Patients: 200
Total Billing: $437.01K
Average Department Billing: $2.19K
Bed Occupancy: 34% (103/~303 total beds)
Average Length of Stay: 4.10 days
Patient Average Age: 47.3 years
Critical Success Factors
Financial Stability: Revenue diversification across diagnosis codes
Operational Efficiency: Optimal bed utilization and length of stay
Quality Care: High discharge rates and appropriate medication management
Strategic Planning: Balanced department utilization with growth opportunities
Industry Benchmarks Comparison
Length of Stay: 4.10 days (meets industry standards)
Bed Occupancy: 34% (conservative but financially sound)
Discharge Rate: High percentage indicates quality care coordination
Revenue per Patient: $2,185 (competitive for community hospital)
These case studies demonstrate how healthcare analytics can drive strategic decision-making, identify operational improvements, and ensure sustainable financial performance while maintaining high-quality patient care.
Turn Your Data Into Decisions
Harness the power of AI, predictive analytics, and real-time processing with Insightlytix. We help businesses unlock insights, scale smarter, and stay ahead of the competition.